RESEARCH PAPER
Qualitative assessment of HIV prevention program on men who have sex with men
in Padang, Indonesia
1
Universitas Andalas, West Sumatra, Indonesia
Submission date: 2022-11-20
Final revision date: 2023-02-09
Acceptance date: 2023-02-09
Online publication date: 2025-08-21
Corresponding author
Mahathir Mahathir
Community Health Nursing, Faculty of Nursing, Universitas Andalas, Padang, Indonesia
Community Health Nursing, Faculty of Nursing, Universitas Andalas, Padang, Indonesia
HIV & AIDS Review 2025;24(3):206-214
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The emerging trend of human immunodeficiency virus (HIV) transmission among men who have sex with men (MSM) is a significant concern in almost all sub-urban cities in Indonesia. The rising number of HIV cases among MSM is similar to an iceberg situation; it will delay the progress of HIV elimination and consequently, alarm healthcare system in the future. This qualitative phenomenological study aimed to review the perceptions of MSM on prevention strategies supporting reduction of the risk of HIV transmission.
Material and methods:
This was a phenomenological research study conducted from July 2021 till January 2022. In-depth interviews took place among a sample of 22 MSM in Padang, Indonesia. Semi-structured questions relating to the insights of participants who engage in HIV transmission risk behaviors, were delivered to all participants. Stevick-Colaizzi-Keen analysis was employed to extract thematic analysis of the study.
Results:
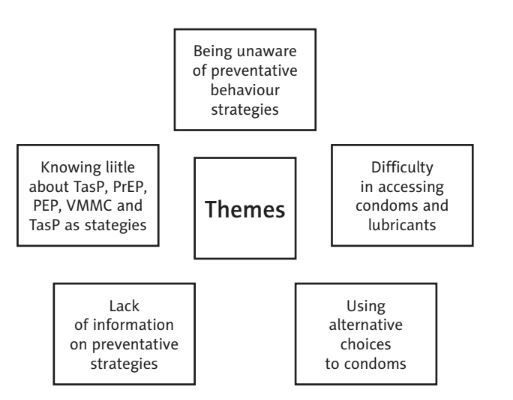
The study found five essential themes, including being unaware of preventative behavior strategies, difficulty in accessing condoms and lubricants, using alternative choices to condoms, lack of information on preventative strategies, and low knowledge about HIV treatment as prevention, pre-exposure antiretroviral prophylaxis, post-exposure antiretroviral prophylaxis, voluntary medical male circumcision, and testing as prevention strategies.
Conclusions:
This study highlights the limitations of the prevention program’s implementation and delivery of information. It is important to provide more appropriate prevention strategies for the MSM population based on their critical areas of need, new evidence, and emerging research on HIV prevention. This will help in a significant long-term reduction of new infection rates.
The emerging trend of human immunodeficiency virus (HIV) transmission among men who have sex with men (MSM) is a significant concern in almost all sub-urban cities in Indonesia. The rising number of HIV cases among MSM is similar to an iceberg situation; it will delay the progress of HIV elimination and consequently, alarm healthcare system in the future. This qualitative phenomenological study aimed to review the perceptions of MSM on prevention strategies supporting reduction of the risk of HIV transmission.
Material and methods:
This was a phenomenological research study conducted from July 2021 till January 2022. In-depth interviews took place among a sample of 22 MSM in Padang, Indonesia. Semi-structured questions relating to the insights of participants who engage in HIV transmission risk behaviors, were delivered to all participants. Stevick-Colaizzi-Keen analysis was employed to extract thematic analysis of the study.
Results:
The study found five essential themes, including being unaware of preventative behavior strategies, difficulty in accessing condoms and lubricants, using alternative choices to condoms, lack of information on preventative strategies, and low knowledge about HIV treatment as prevention, pre-exposure antiretroviral prophylaxis, post-exposure antiretroviral prophylaxis, voluntary medical male circumcision, and testing as prevention strategies.
Conclusions:
This study highlights the limitations of the prevention program’s implementation and delivery of information. It is important to provide more appropriate prevention strategies for the MSM population based on their critical areas of need, new evidence, and emerging research on HIV prevention. This will help in a significant long-term reduction of new infection rates.
REFERENCES (48)
1.
United Nations Sustainable Development Group. Operationalizing Leaving No One Behind. 2022. Available at: https://unsdg.un.org/resources....
2.
UNAIDS. Global AIDS Strategy 2021-2026 [Internet]. 2021. Available at: https://www.unaids.org/sites/d... (Accessed: 09.09.2023).
3.
Gottlieb MS, Schroff R, Schanker HM, Weisman JD, Fan PT, Wolf RA, et al. Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency. N Engl J Med 1981; 305: 1425-1431.
4.
UNAIDS. Key populations. Vol. 1, UNAIDS Report. 2016. Available at: https://open.unaids.org/sites/....
5.
UNAIDS. UNAIDS Global AIDS Update [Internet]. 2022. Available at: https://www.unaids.org/sites/d... (Accessed: 09.11.2022).
6.
UNAIDS. 2025 AIDS TARGETS [Internet]. 2021. Available at: https://www.unaids.org/sites/d... (Accessed: 09.02.2023).
7.
Verboom B, Melendez-Torres G, Bonell CP. Combination methods for HIV prevention in men who have sex with men (MSM). Cochrane Database Syst Rev 2018; 2018: CD010939. DOI: 10.1002/CD010939.pub2.
8.
Unaids. Fact Sheet 2022 [Internet]. 2021. Available at: https://www.unaids.org/sites/d... (Accessed: 09.09.2023).
9.
UNAIDS. Confronting inequalities: lessons for pandemic responses from 40 years of AIDS. 2021. Geneva: UNAIDS; 2021.
10.
Biello KB, Mimiaga MJ, Santostefano CM, Novak DS, Mayer KH. MSM at highest risk for HIV acquisition express greatest interest and preference for injectable antiretroviral PrEP compared to daily, oral medication. AIDS Behav 2018; 22: 1158-1164.
11.
Kementerian Kesehatan & UNICEF. Integrated Biological-Behavioral Surveillance Survey Among Adolescent and Young People Who Inject Drugs, Female Sex Workers, Males Who Have Sex with Males and Male to Female Transgender Persons [Internet]. 2018. Available at: https://www.unicef.org/indones... (Accessed: 09.12.2023).
12.
Dirjen P2p Kemenkes RI. Laporan Perkembangan HIV/AIDS dan Penyakit Infeksi Menular Seksual Tahun 2021 [Internet]. 2021. Available at: https://siha.kemkes.go.id/port... (Accessed: 19.10.2023).
13.
Dinas Kesehatan Kota Padang. Laporan Tahunan Dinas Kesehatan Kota Padang [Internet]. 2021. Available at: https://dinkes.padang.go.id/la... (Accessed: 09.09.2023).
14.
Dinas Kesehaatn Kota Padang. Profil Kesehatan Tahun 2019 [Internet]. 2019. Available at: https://ppid.padang.go.id/uplo... (Accessed: 12.11.2023).
15.
Baral S, Sifakis F, Cleghorn F, Beyrer C, Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000-2006: a systematic review. PLoS Med 2007; 4: e339. DOI: 10.1371/journal.pmed.0040339.
16.
Dong MJ, Peng B, Liu ZF, Ye QN, Liu H, Lu XL, et al. The prevalence of HIV among MSM in China: a large-scale systematic analysis. BMC Infect Dis 2019; 19: 1000. DOI: 10.1186/s12879-019-4559-1.
17.
Babel RA, Wang P, Alessi EJ, Raymond HF, Wei C. Stigma, HIV risk, and access to HIV prevention and treatment services among men who have sex with men (MSM) in the United States: a scoping review. AIDS Behav 2021; 25: 3574-3604.
18.
Zheng M, He J, Yuan Z, Zhang X, Yao Y, Fang X, et al. Risk assessment and identification of HIV infection among men who have sex with men: a cross-sectional study in Southwest China. BMJ Open 2020; 10: e039557. DOI: 10.1136/bmjopen-2020-039557.
19.
Gedela K, Januraga PP, Luis H, Wignall FS, Irwanto I. COVID-19 lockdown in Indonesia: greater investment will be needed to mitigate the impact on people living with HIV. Asia Pac J Public Health 2020; 32: 461-462.
20.
Nevendorff L, Schroeder SE, Pedrana A, Bourne A, Stoové M. Prevalence of sexualized drug use and risk of HIV among sexually active MSM in East and South Asian countries: systematic review and meta-analysis. J Int AIDS Soc 2023; 26: 26054. DOI: 10.1002/jia2.26054.
21.
Threats M, Brawner BM, Montgomery TM, Abrams J, Jemmott LS, Crouch PC, et al. A review of recent HIV prevention interventions and future considerations for nursing science. J Assoc Nurses AIDS Care 2021; 32: 373-391.
22.
Kementerian Kesehatan. Program Pengendalian HIV AIDS dan PIMS [Internet]. 2017 [cited 2022 Nov 29]. Available at: https://siha.kemkes.go.id/port....
23.
Mnyaka OR, Mabunda SA, Chitha WW, Nomatshila SC, Ntlongweni X. Barriers to the implementation of the HIV universal test and treat strategy in selected primary care facilities in South Africa’s Eastern Cape povince. J Prim Care Community Health 2021; 12: 21501327211028706. DOI: 10.1177/21501327211028706.
24.
Fields EL, Hussen SA, Malebranche DJ. Mind the gap: HIV prevention among young black men who have sex with men. Curr HIV AIDS Rep 2020; 17: 632-642.
25.
Veronese V, Clouse E, Wirtz AL, Thu KH, Naing S, Baral SD, et al. “We are not gays... don’t tell me those things”: Engaging “hidden” men who have sex with men and transgender women in HIV prevention in Myanmar. BMC Public Health 2019; 19: 63. DOI: 10.1186/s12889-018-6351-3.
26.
Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 2013.
27.
Tongco C Dolores Ma. Purposive Sampling as a Tool for Informant Selection. University Hawaii. 2017.
28.
Hardisman Dasman. Perilaku LSL dan Penularan HIV AIDS di Sumbar Paradoks Sosial di Minangkabau [Internet]. 2018. Available at: http://repo.unand.ac.id/6643/1... (Accessed: 12.12.2022).
29.
Hess KL, Crepaz N, Rose C, Purcell D, Paz-Bailey G. Trends in sexual behavior among men who have sex with men (MSM) in high-income countries, 1990-2013: a systematic review. AIDS Behav 2017; 21: 2811-2834.
30.
Vagenas P, Ludford KT, Gonzales P, Peinado J, Cabezas C, Gonzales F, et al. Being unaware of being HIV-Infected is associated with alcohol use disorders and high-risk sexual behaviors among men who have sex with men in Peru. AIDS Behav 2014; 18: 120-127.
31.
Nakiganda LJ, Bell S, Grulich AE, Serwadda D, Nakubulwa R, Poynten IM, et al. Understanding and managing HIV infection risk among men who have sex with men in rural Uganda: a qualitative study. BMC Public Health 2021; 21: 1309. DOI: 10.1186/s12889-021-11365-9.
32.
Iott BE, Loveluck J, Benton A, Golson L, Kahle E, Lam J, et al. The impact of stigma on HIV testing decisions for gay, bisexual, queer and other men who have sex with men: a qualitative study. BMC Public Health 2022; 22: 471. DOI: 10.1186/s12889-022-12761-5.
33.
Bekker LG, Alleyne G, Baral S, Cepeda J, Daskalakis D, Dowdy D, et al. Advancing global health and strengthening the HIV response in the era of the Sustainable Development Goals: the International AIDS Society – Lancet Commission. Lancet 2018; 392: 312-358.
34.
Sharma A, Paredes-Vincent A, Kahle EM. Awareness, utilization, and preferences for traditional and contemporary HIV prevention strategies among Facebook and Instagram-using MSM in the United States. J Int Assoc Provid AIDS Care 2021; 20: 23259582211024770. DOI: 10.1177/23259582211024770.
35.
Reza MM, Rana AKMM, Azim T, Chowdhury EI, Gourab G, Imran MS, et al. Changes in condom use among males who have sex with males (MSM): Measuring the effect of HIV prevention programme in Dhaka city. PLoS One 2020; 15: e0236557. DOI: 10.1371/journal.pone.0236557.
36.
Restar AJ, Adia A, Nazareno J, Hernandez L, Sandfort T, Lurie M, et al. Barriers and facilitators to uptake of condoms among Filipinx transgender women and cisgender men who have sex with men: a situated socio-ecological perspective. Glob Public Health 2020; 15: 520-531.
37.
Pines HA, Patrick R, Smith DM, Harvey-Vera A, Blumenthal JS, Rangel G, et al. HIV prevention method preferences within sexual partnerships reported by HIV-negative MSM and TW in Tijuana, Mexico. AIDS Behav 2020; 24: 839-846.
38.
Mansergh G, Kiran Kota K, Stephenson R, Hirshfield S, Sullivan P. Preference for using a variety of future HIV pre-exposure prophylaxis products among men who have sex with men in three US cities. J Int AIDS Soc 2021; 24: e25664. DOI: 10.1002/jia2.25664.
39.
Mahathir M, Wiarsih W, Permatasari H. How do people living with HIV acquire HIV related information: a qualitative evaluation of Jakarta setting. J Ners 2020; 15: 126-134.
40.
Liu Z, Chen Y, Yao T, Zhang T, Song D, Liu Y, et al. Factors related to HIV testing frequency in MSM based on the 2011-2018 survey in Tianjin, China: a hint for risk reduction strategy. BMC Public Health 2021; 21: 1900. DOI: 10.1186/s12889-021-11948-6.
41.
Thanavanh B, Harun-Or-Rashid M, Kasuya H, Sakamoto J. Knowledge, attitudes and practices regarding HIV/AIDS among male high school students in Lao People’s Democratic Republic. J Int AIDS Soc 2013; 16: 17387. DOI: 10.7448/IAS.16.1.17387.
42.
Guimarães MDC, Magno L, Ceccato MDGB, Gomes RR de FM, Leal AF, Knauth DR, et al. HIV/AIDS knowledge among MSM in Brazil: A challenge for public policies. Rev Bras Epidemiol 2019; 22 (Suppl 1): e190005. DOI: 10.1590/1980-549720190005.supl.1.
43.
van Griensven F, Guadamuz TE, de Lind van Wijngaarden JW, Phanuphak N, Solomon SS, Lo YR. Challenges and emerging opportunities for the HIV prevention, treatment and care cascade in men who have sex with men in Asia Pacific. Sex Transm Infect 2017; 93: 356-362.
44.
Bor J, Fischer C, Modi M, Richman B, Kinker C, King R, et al. Changing knowledge and attitudes towards HIV treatment-as-prevention and “undetectable = untransmittable”: a systematic review. AIDS Behav 2021; 25: 4209-4224.
45.
Torres TS, de Boni RB, de Vasconcellos MTL, Luz PM, Hoagland B, Moreira RI, et al. Awareness of prevention strategies and willingness to use preexposure prophylaxis in brazilian men who have sex with men using apps for sexual encounters: online cross-sectional study. JMIR Public Health Surveill 2018; 4: e11. DOI: 10.2196/publichealth.8997.
46.
Bekker LG, Pike C, Hillier SL. HIV prevention: better choice for better coverage. J Int AIDS Soc 2022; 25: e25872. DOI: 10.1002/jia2.25872.
47.
Gilmour S, Peng L, Li J, Oka S, Tanuma J. New strategies for prevention of HIV among Japanese men who have sex with men: a mathematical model. Sci Rep 2020; 10: 18187. DOI: 10.1038/s41598-020-75182-7.
48.
Yuan T, Fitzpatrick T, Ko NY, Cai Y, Chen Y, Zhao J, et al. Circumcision to prevent HIV and other sexually transmitted infections in men who have sex with men: a systematic review and meta-analysis of global data. Lancet Glob Health 2019; 7: e436-e447. DOI: 10.1016/S2214-109X(18)30567-9.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.