RESEARCH PAPER
Views on HIV self-testing among adolescent and young men who have sex with men and transgender people in Bangladesh: a qualitative exploration to inform HIV program
1
UNAIDS, Bangladesh
2
Department of Statistics and Data Science, Jahangirnagar University, Savar, Dhaka, Bangladesh
3
Bandhu Social Welfare Society (Bandhu), Bangladesh
4
UNFPA, Bangladesh
Submission date: 2023-01-04
Final revision date: 2023-03-27
Acceptance date: 2023-03-28
Publication date: 2025-09-07
Corresponding author
Sabina Yasmin
Department of Statistics and Data Science, Jahangirnagar University, Savar, Dhaka 1342, Bangladesh
Department of Statistics and Data Science, Jahangirnagar University, Savar, Dhaka 1342, Bangladesh
HIV & AIDS Review 2025;24(3):224-233
KEYWORDS
TOPICS
ABSTRACT
Introduction:
In Bangladesh, human immunodeficiency virus (HIV) testing coverage needs to increase in general. Traditional HIV testing services are yet to attract underprivileged and vulnerable populations, such as men who have sex with men (MSM) and transgender (TG/hijra) people. For this purpose, priority should be given to communities, who are less aware of availability of HIV self-testing (HIVST). This study aimed to understand the awareness, willingness to perform HIVST, and preferred choices and views of young and adolescent MSM and TGs regarding HIV infection, and the proposed opportunity of HIV self-testing with risk perceptions.
Material and methods:
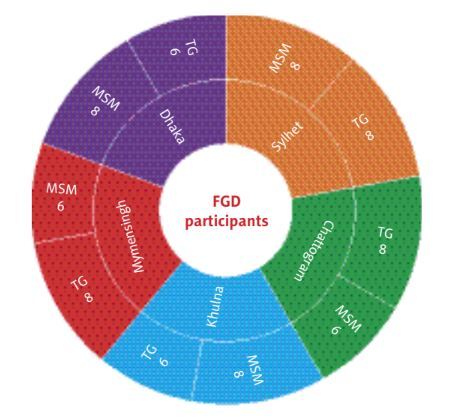
The study used a convenience sampling methodology to recruit participants among young MSM and TGs through Health Initiatives for Men (HIM) centers in Bangladesh. In each study site, one focus group discussion (FGD) was conducted with each target group; there were 10 FGDs in five study sites, and 72 FGD participants in total.
Results:
The study findings revealed that, despite a poor awareness level, HIV self-testing by oral fluid was well-accepted among the young MSM and TGs. The majority of FGD participants preferred an oral saliva testing kit with assisted testing services. They also suggested to assess cost-effectiveness of various HIVST distribution strategies, ensuring pre- and post-test counseling, referral for a confirmatory test (facility-based), and link with an antiretroviral center if needed.
Conclusions:
HIVST has the potential to strongly impact rapid scaling-up of existing testing procedures. Therefore, collaboration between government and community stakeholders is required to identify the most optimal strategies of HIVST implementation, considering cost-effectiveness of HIVST kits.
In Bangladesh, human immunodeficiency virus (HIV) testing coverage needs to increase in general. Traditional HIV testing services are yet to attract underprivileged and vulnerable populations, such as men who have sex with men (MSM) and transgender (TG/hijra) people. For this purpose, priority should be given to communities, who are less aware of availability of HIV self-testing (HIVST). This study aimed to understand the awareness, willingness to perform HIVST, and preferred choices and views of young and adolescent MSM and TGs regarding HIV infection, and the proposed opportunity of HIV self-testing with risk perceptions.
Material and methods:
The study used a convenience sampling methodology to recruit participants among young MSM and TGs through Health Initiatives for Men (HIM) centers in Bangladesh. In each study site, one focus group discussion (FGD) was conducted with each target group; there were 10 FGDs in five study sites, and 72 FGD participants in total.
Results:
The study findings revealed that, despite a poor awareness level, HIV self-testing by oral fluid was well-accepted among the young MSM and TGs. The majority of FGD participants preferred an oral saliva testing kit with assisted testing services. They also suggested to assess cost-effectiveness of various HIVST distribution strategies, ensuring pre- and post-test counseling, referral for a confirmatory test (facility-based), and link with an antiretroviral center if needed.
Conclusions:
HIVST has the potential to strongly impact rapid scaling-up of existing testing procedures. Therefore, collaboration between government and community stakeholders is required to identify the most optimal strategies of HIVST implementation, considering cost-effectiveness of HIVST kits.
REFERENCES (35)
1.
UNAIDS. 2025 AIDS targets. 2020. Available from: https://aidstargets2025.unaids... (Accessed: 05.03.2022).
2.
Johnson C, Baggaley R, Forsythe S, van Rooyen H, Ford N, Napierala Mavedzenge S, et al. Realizing the potential for HIV self-testing. AIDS Behav 2014; 18: 391-395.
3.
UNAIDS. Global AIDS Update 2018 Miles To Go: Closing Gaps Breaking Barriers Righting Injustices. Unaids. 2018. Available from: http://www.unaids.org/sites/de... (Accessed: 07.03.2022).
4.
UNAIDS. Data 2020. Program HIV/AIDS. 2020. Available from: https://www.unaids.org/en/reso... (Accessed: 07.03.2022).
5.
National AIDS/STD Program. 3rd National Strategic Plan for HIV and AIDS Response in Bangladesh, 2011-2015. 2011. Available from: https://www.aidsdatahub.org/re... (Accessed: 07.03.2022).
6.
Chan PA, Khan OA. Risk factors for HIV infection in Males who have Sex with Males (MSM) in Bangladesh. BMC Public Health 2007; 7: 153. DOI: https://doi.org/10.1186/1471-2....
7.
MOHFW. World AIDS Day 2020: HIV/AIDS Situation in Bangladesh. 2020. Available from: http://asp.portal.gov.bd/sites....
8.
Joint United Nations Programme on HIV/AIDS (UNAIDS). AIDS data 2019 [Internet]. Vol. 268, Science. 2019. Available from: https://www.unaids.org/en/reso....
9.
WHO. HIV and young men who have sex with men. Technical Brief. 2015. Available from: http://apps.who.int/iris/bitst....
10.
Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Manseau MW, Montenegro AB, et al. Depressive symptoms, utilization of ental health care, substance use and sexual risk among young Men who have sex with men in explore: Implications for age-specific interventions. AIDS Behav 2009; 13: 811-821.
11.
Shafik N, Deeb S, Srithanaviboonchai K, Ayood P, Malasao R, Siviroj P, et al. Awareness and attitudes toward HIV self-testing in northern Thailand. Int J Environ Res Public Health 2021; 18: 852. DOI: 10.3390/ijerph18030852.
12.
Hamilton A, Shin S, Taggart T, Whembolua GL, Martin I, Budhwani H, et al. HIV testing barriers and intervention strategies among men, transgender women, female sex workers and incarcerated persons in the Caribbean: a systematic review. Sex Transm Infect 2020; 96: 189-196.
13.
Johnston LG, Steinhaus MC, Sass J, Sirinirund P, Lee C, Benjarattanaporn P, et al. Recent HIV testing among young men who have sex with men in Bangkok and Chiang Mai: HIV testing and prevention strategies must be enhanced in Thailand. AIDS Behav 2016; 20: 2023-2032.
14.
World Health Organization. Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services. 2016. Available from: https://apps.who.int/iris/hand....
15.
WHO. Asia-Pacific countries meet to progress PrEP and HIV self-testing. 2019. Available from: https://www.who.int/hiv/events....
16.
Asian Network of People Living with HIV/AIDS (APN+): Improving Community-Based/Led HIV Testing Services Among Transgender People and People Who Inject Drugs in Asia: Desk Review Report. 2019. Available from: http://www.apnplus.org/?p=1471.
17.
Hlongwa M, Hlongwana K, Makhunga S, Choko AT, Dzinamarira T, Conserve D, et al. Linkage to HIV care following HIV self-testing among men: systematic review of quantitative and qualitative studies from six countries in sub-Saharan Africa. AIDS Behav 2022; 27: 651-666.
18.
Rao A, Patil S, Aheibam S, Kshirsagar P, Hemade P, Panda S. Acceptability of HIV oral self-test among men having sex with men and transgender population: a qualitative investigation from Pune, India. Infect Dis (Auckl) 2020; 13: 117863372096280. DOI: 10.1177/1178633720962809.
19.
Girault P, Wong CM, Jittjang S, Fongkaew K, Cassell MM, Lertpiriyasuwat C, et al. Uptake of oral fluid-based HIV self-testing among men who have sex with men and transgender women in Thailand. PLoS One 2021; 16: e0256094. DOI: 10.1371/journal.pone.0256094.
20.
Figueroa C, Johnson C, Verster A, Baggaley R. Attitudes and acceptability on HIV self-testing among key populations: a literature review. AIDS Behav 2015; 19: 1949-1965.
21.
Volk JE, Lippman SA, Grinsztejn B, Lama JR, Fernandes NM, Gonzales P, et al. Acceptability and feasibility of HIV self-testing among men who have sex with men in Peru and Brazil. Int J STD AIDS 2016; 27: 531-536.
22.
Zanolini A, Chipungu J, Vinikoor MJ, Bosomprah S, Mafwenko M, Holmes CB, et al. HIV self-testing in Lusaka Province, Zambia: acceptability, comprehension of testing instructions, and individual preferences for self-test kit distribution in a population-based sample of adolescents and adults. AIDS Res Hum Retroviruses 2018; 34: 254-260.
23.
Bustamante MJ, Konda KA, Joseph Davey D, León SR, Calvo GM, Salvatierra J, et al. HIV self-testing in Peru: questionable availability, high acceptability but potential low linkage to care among men who have sex with men and transgender women. Int J STD AIDS 2016; 28: 133-137.
24.
Altaf A, Pasha MSK, Majeed A, Ali W, Alaama AS, Jamil MS. Acceptability and feasibility of HIV self-testing among transgender people in Larkana, Pakistan: results from a pilot project. PLoS One 2022; 17: e0270857. DOI: 10.1371/journal.pone.0270857.
25.
Moradi G, Amini EE, Valipour A, Tayeri K, Kazerooni PA, Molaeipour L, et al. The study of feasibility and acceptability of using HIV self-tests in high-risk Iranian populations (FSWs, MSM, and TGs): a cross-sectional study. Harm Reduct J 2022; 19: 61. DOI: 10.1186/s12954-022-00641-5.
26.
Cassell MM, Girault P, Nith S, Rang C, Sokhan S, Tuot S, et al. A cross-sectional assessment of HIV self-testing preferences and uptake among key populations in Phnom Penh, Cambodia. Glob Heal Sci Pract 2022; 10: e2100412. DOI: 10.9745/GHSP-D-21-00412.
27.
Lyons CE, Coly K, Bowring AL, Liestman B, Diouf D, Wong VJ, et al. Use and acceptability of HIV Self-testing among first-time testers at risk for HIV in Senegal. AIDS Behav 2019; 23 (Suppl 2): 130-141.
28.
van Dyk AC. Client-initiated, provider-initiated, or self-testing for HIV: what do South Africans prefer? J Assoc Nurses AIDS Care 2013; 24: e45-e56. DOI: 10.1016/j.jana.2012.12.005.
29.
Kurth AE, Cleland CM, Chhun N, Sidle JE, Were E, Naanyu V, et al. Accuracy and acceptability of oral fluid HIV self-testing in a general adult population in Kenya. AIDS Behav 2016; 20: 870-879.
30.
Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature 2015; 528: S77-S85.
31.
Hector J, Davies MA, Dekker-Boersema J, Aly MM, Abdalad CCA, Langa EBR, et al. Acceptability and performance of a directly assisted oral HIV self-testing intervention in adolescents in rural Mozambique. PLoS One 2018; 13: e0195391. DOI: 10.1371/journal.pone.0195391.
32.
Pal K, Ngin C, Tuot S, Chhoun P, Ly C, Chhim S, et al. Acceptability study on HIV self-testing among transgender women, men who have sex with men, and female entertainment workers in Cambodia: a qualitative analysis. PLoS One 2016; 11: e0166129. DOI: 10.1371/journal.pone.0166129.
33.
Mokgatle MM, Madiba S. High acceptability of HIV self-testing among technical vocational education and training college students in Gauteng and North West Province: what are the implications for the scale up in South Africa? PLoS One 2017; 12: e0169765. DOI: 10.1371/journal.pone.0169765.
34.
Madiba S, Segobola M, Mokgatle M. Assessing the acceptability and willingness to use HIV self-testing among student nurses in a Private Nursing College, Gauteng Province, South Africa. World J AIDS 2015; 5: 208-216.
35.
Estem KS, Catania J, Klausner JD. HIV self-testing: a review of current implementation and fidelity. Curr HIV AIDS Rep 2016; 13: 107-115.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.