RESEARCH PAPER
The impact of comprehensive sexuality education on promoting safe sexual behaviors among 15-24 year-old youths with HIV
1
Department of Midwifery and Reproductive Health, Faculty of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
2
Department of Infectious Diseases, Tehran University of Medical Science, Tehran, Iran
3
Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran
4
Department of Public Health Nursing, Nursing Faculty, Aja University of Medical Sciences, Tehran, Iran
5
Research Center for Cancer Screening and Epidemiology, Aja University of Medical Sciences, Tehran, Iran
6
Counseling and Reproductive Health Research Center, Department of Midwifery, Faculty of Nursing and Midwifery, Golestan University of Medical Sciences (GOUMS), Gorgan, Iran
7
Student Research Committee, School of Nursing and Midwifery, Shahroud University of Medical Sciences, Shahroud, Iran
8
Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Submission date: 2023-09-26
Final revision date: 2023-10-25
Acceptance date: 2023-10-30
Online publication date: 2025-11-20
Corresponding author
Zahra Behboodi Moghadam
Department of Midwifery and Reproductive Health,Faculty of Nursing and Midwifery,Tehran University of Medical Sciences,Tehran,Iran
Department of Midwifery and Reproductive Health,Faculty of Nursing and Midwifery,Tehran University of Medical Sciences,Tehran,Iran
HIV & AIDS Review 2025;24(4):290-296
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Many people in different societies regard the topic of sexual needs important, but it is not considered in health service packages nor included in patients’ evaluation. Therefore, the purpose of this study was to investigate the effect of a comprehensive sexuality education (CSE) program on the promotion of safe sexual behaviors among human immunodeficiency virus (HIV)-positive youths aged 15-24 years.
Material and methods:
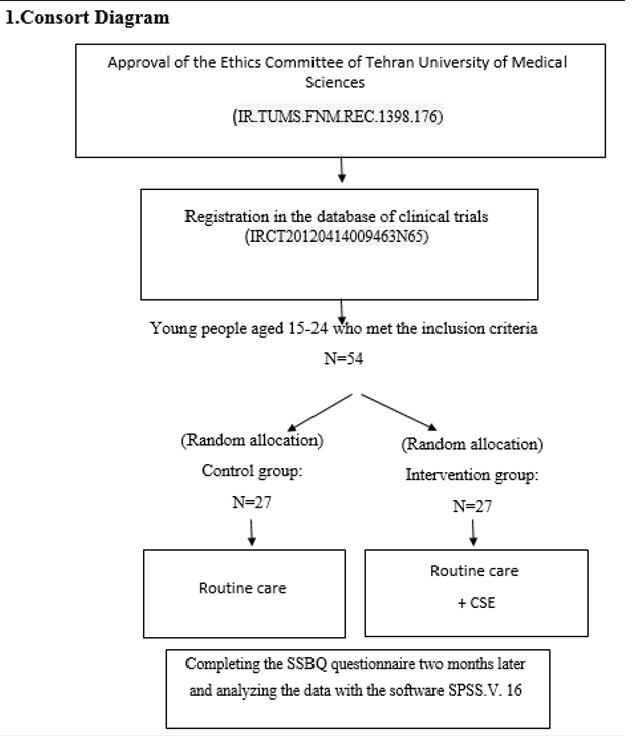
This study was a clinical trial with both intervention and control groups, with 27 HIV-infected adolescences aged 15 to 24 years enrolled in each group. Data collection tool was a questionnaire consisting of three sections, i.e., demographics characteristics and history and status of the disease as well as standard safe sexual behavior questionnaire (SSBQ) was used. Five training sessions were conducted, which were held in groups of 2-5 people, with each session lasting for about 60-90 minutes. Respondents completed SSBQ before and two months after the intervention.
Results:
The results of data analysis indicated that CSE has improved the overall score of safe sexual behavior among the intervention group members (p = 0.001). In the sub-fields of protective behavior, such as avoiding high-risk sexual behavior and avoiding sexual partner's secretions and fluids, there was a significant positive effect but not statistically significant effect in the sub-field of inter-personal skills was observed.
Conclusions:
By implementing the CSE program among HIV-infected youths, positive effects can be expected in promoting safe sexual behaviors. It is suggested to employ CSE in educational programs of adolescences.
Many people in different societies regard the topic of sexual needs important, but it is not considered in health service packages nor included in patients’ evaluation. Therefore, the purpose of this study was to investigate the effect of a comprehensive sexuality education (CSE) program on the promotion of safe sexual behaviors among human immunodeficiency virus (HIV)-positive youths aged 15-24 years.
Material and methods:
This study was a clinical trial with both intervention and control groups, with 27 HIV-infected adolescences aged 15 to 24 years enrolled in each group. Data collection tool was a questionnaire consisting of three sections, i.e., demographics characteristics and history and status of the disease as well as standard safe sexual behavior questionnaire (SSBQ) was used. Five training sessions were conducted, which were held in groups of 2-5 people, with each session lasting for about 60-90 minutes. Respondents completed SSBQ before and two months after the intervention.
Results:
The results of data analysis indicated that CSE has improved the overall score of safe sexual behavior among the intervention group members (p = 0.001). In the sub-fields of protective behavior, such as avoiding high-risk sexual behavior and avoiding sexual partner's secretions and fluids, there was a significant positive effect but not statistically significant effect in the sub-field of inter-personal skills was observed.
Conclusions:
By implementing the CSE program among HIV-infected youths, positive effects can be expected in promoting safe sexual behaviors. It is suggested to employ CSE in educational programs of adolescences.
REFERENCES (58)
1.
Karbasian P, Kalantari F. The determination of young couples educational needs in Yazd. Toloo-e-behdasht 2014; 2: 113-127. Available at: https://doaj.org/article/03941... 2b9b7.
2.
Hetrick SE, Bailey AP, Smith KE, Malla A, Mathias S, Singh SP, et al. Integrated (one‐stop shop) youth health care: Best available evidence and future directions. Med J Aust 2017; 207 (S10): S5-S18. DOI: 10.5694/mja17.00694.
3.
International Conference on Population and Development. Available at: https://www.unfpa.org/icpd.
4.
Dowshen N, D’Angelo L. Health care transition for youth living with HIV/AIDS. Pediatrics 2011; 128: 762-771.
5.
Cottingham J. Sexual and reproductive: connections and disconnections in public health. In: Aggleton P, Parker R (eds.). Routledge Handbook of Sexuality, Health And Rights. Routledge; 2010, p. 167-74.
6.
Fatusi AO, Hindin MJ. Adolescents and youth in developing countries: health and development issues in context. J Adolesc 2010; 33: 499-508.
8.
UNAIDS. Global HIV & AIDS statistics – fact sheet. Available at: https://www.unaids.org/en/reso....
9.
UNAIDS. Youth and HIV – mainstreaming a three-lens approach to youth participation. Available at: https://wwwunaidsorg/sites/def.... 2018.
13.
Trickey A, May MT, Vehreschild JJ, Obel N, Gill MJ, Crane HM, et al. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV 2017; 4: e349-e356. DOI: 10.1016/S2352-3018- (17)30066-8.
14.
Nsanzimana S, Remera E, Kanters S, Chan K, Forrest JI, Ford N, et al. Life expectancy among HIV-positive patients in Rwanda: a retrospective observational cohort study. Lancet Glob Health 2015; 3: e169-e177. DOI: 10.1016/S2214-109X(14)70364-X.
15.
Bennett DS, Hersh J, Herres J, Foster J. HIV-related stigma, shame, and avoidant coping: Risk factors for internalizing symptoms among youth living with HIV? Child Psychiatry Hum Dev 2016; 47: 657-664.
16.
Rongkavilit C, Wright K, Chen X, Naar-King S, Chuenyam T, Phanuphak P. HIV stigma, disclosure and psychosocial distress among Thai youth living with HIV. Int J STD AIDS 2010; 21: 126-132.
17.
Darrow WW, Montanea JE, Gladwin H. AIDS-related stigma among Black and Hispanic young adults. AIDS Behav 2009; 13: 1178-1188.
18.
Majumdar B, Mazaleni N. The experiences of people living with HIV/AIDS and of their direct informal caregivers in a resource-poor setting. J Int AIDS Soc 2010; 13: 20. DOI: 10.1186/1758-2652- 13-20.
19.
Avci D, Dogan S. The Impact of sexual dysfunction on quality of life of patients with asthma in Turkey. Sex Disabil 2017; 35: 107-118.
20.
Nesamoney SN, Mejía-Guevara I, Cislaghi B, Weber AM, Mbizvo MT, Darmstadt GL. Social normative origins of the taboo gap and implications for adolescent risk for HIV infection in Zambia. Soc Sci Med 2022; 312: 115391. DOI: 10.1016/j.socscimed.2022.115391.
21.
Vujovic M, Struthers H, Meyersfeld S, Dlamini K, Mabizela N. Addressing the sexual and reproductive health needs of young adolescents living with HIV in South Africa. Children and Youth Services Review 2014; 45: 122-128.
22.
Akre C, Berchtold A, Gmel G, Suris JC. The evolution of sexual dysfunction in young men aged 18-25 years. J Adolesc Health 2014; 55: 736-743.
23.
Varghese KM, Bansal R, Kekre AN, Jacob K. Sexual dysfunction among young married women in southern India. Int Urogynecol J 2012; 23: 1771-1774.
24.
Du J, Ruan X, Gu M, Bitzer J, Mueck AO. Prevalence of and risk factors for sexual dysfunction in young Chinese women according to the Female Sexual Function Index: an internet-based survey. Eur J Contracept Reprod Health Care 2016; 21: 259-263.
25.
Moreau C, Kågesten AE, Blum RW. Sexual dysfunction among youth: an overlooked sexual health concern. BMC Public Health 2016; 16: 1170. DOI: 10.1186/s12889-016-3835-x.
26.
Wang Q, Young J, Bernasconi E, Cavassini M, Vernazza P, Hirschel B, et al. The prevalence of erectile dysfunction and its association with antiretroviral therapy in HIV-infected men: the Swiss HIV Cohort Study. Antivir Ther 2013; 18: 337-344.
27.
Shindel AW, Horberg MA, Smith JF, Breyer BN. Sexual dysfunction, HIV, and AIDS in men who have sex with men. AIDS Patient Care STDs 2011; 25: 341-349.
28.
Asadi L, Ziaei T, Koochak HE, Montazeri A, Rezaei E, Moghadam ZB, et al. Effect of counseling based on PLISSIT model on sexual function of HIV-positive married women. HIV AIDS Rev 2018; 17: 169-175.
29.
Behboodi Moghadam Z, Rezaei E, Yalegonbadi K, Montazeri A, Arzaqi SM, Tavakol Z, et al. The effect of sexual health education program on women sexual function in Iran. J Res Health Sci 2015; 15: 124-128.
30.
Rijsdijk LE, Bos AE, Ruiter RA, Leerlooijer JN, de Haas B, Schaal-ma HP. The World Starts With Me: A multilevel evaluation of a comprehensive sex education programme targeting adolescents in Uganda. BMC Public Health 2011; 11: 334. DOI: 10.1186/14712458-11-334.
31.
Witwer E, Jones R, Lindberg L. Sexual behavior and contraceptive and condom use among U.S. high school students, 2013-2017. New York: Guttmacher Institute; 2018. DOI: https://doi.org/10.1363/2018.2....
32.
Muchiri E, Odimegwu C, De Wet N. HIV risk perception and consistency in condom use among adolescents and young adults in urban Cape Town, South Africa: a cumulative risk analysis. Southern Afr J Infect Dis 2017; 32: 105-110.
33.
Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, et al. South African national HIV prevalence, incidence and behaviour survey, 2012. Cape Town: HSRC Press; 2014.
34.
Rana Y, Brown RA, Kennedy DP, Ryan GW, Stern S, Tucker JS. Understanding condom use decision making among homeless youth using event-level data. J Sex Res 2015; 52: 1064-1074.
35.
Higgins JA, Gregor L, Mathur S, Nakyanjo N, Nalugoda F, Santel-li JS. Use of withdrawal (coitus interruptus) for both pregnancy and HIV prevention among young adults in Rakai, Uganda. J Sex Med 2014; 11: 2421-2427.
36.
Brown RA, Kennedy DP, Tucker JS, Wenzel SL, Golinelli D, Wertheimer SR, et al. Sex and relationships on the street: How homeless men judge partner risk on Skid Row. AIDS Behav 2012; 16: 774-784.
37.
Chanakira E, O’Cathain A, Goyder EC, Freeman JV. Factors perceived to influence risky sexual behaviours among university students in the United Kingdom: a qualitative telephone interview study. BMC Public Health 2014; 14: 1055. DOI: 10.1186/1471-2458-14-1055.
38.
Chawla N, Sarkar S. Defining “high-risk sexual behavior” in the context of substance use. J Psychosex Health 2019; 1: 26-31.
39.
Dimbuene ZT, Defo BK. Risky sexual behaviour among unmarried young people in Cameroon: another look at family environment. J Biosoc Sci 2011; 43: 129-153.
40.
Mutinta G, Govender K, Gow J, George G. An investigation on students’ risky sexual behavior at KwaZulu-Natal University, Durban, South Africa. Am J Sex Educ 2013; 8: 121-139.
41.
Mirzaei M, Ahmadi K, Saadat SH, Ramezani MA. Instruments of high risk sexual behavior assessment: a systematic review. Mater Sociomed 2016; 28: 46-50.
42.
Agajie M, Belachew T, Tilahun T, Amentie M. Risky sexual behavior and associated factors among high school youth in Pawe Woreda, Benishangul Gumuz Region. Sci J Clin Med 2015; 4: 67-75.
43.
Valdes B, Gattamorta K, Jones SG, Fenkl EA, De Santis JP. Social support, loneliness, depressive symptoms, and high-risk sexual behaviors of middle-aged Hispanic men who have sex with men. J Assoc Nurses AIDS Care 2019; 30: 98-110.
44.
Stanger-Hall KF, Hall DW. Abstinence-only education and teen pregnancy rates: why we need comprehensive sex education in the US. PLoS One 2011; 6: e24658. DOI: 10.1371/journal.pone.0024658.
45.
Fonner VA, Armstrong KS, Kennedy CE, O’Reilly KR, Sweat MD. School based sex education and HIV prevention in low-and middle-income countries: a systematic review and meta-analysis. PLoS One 2014; 9: e89692. DOI: 10.1371/journal.pone.0089692.
46.
Anglewicz P, Clark S. The effect of marriage and HIV risks on condom use acceptability in rural Malawi. Soc Sci Med 2013; 97: 29-40.
47.
Breuner CC, Mattson G; Committee on Adolescence; Committee on Psychosocial Aspects of Child and Family Health. Sexuality education for children and adolescents. Pediatrics 2016; 138: e20161348. DOI: 10.1542/peds.2016-1348.
48.
Coyle K, Anderson P, Laris B. Schools and sexuality education. In: Ponzetti JJ Jr. (ed.). Evidence-based Approaches to Sexuality Education. Routledge; 2015, p. 170-192.
49.
Lameiras-Fernández M, Martínez-Román R, Carrera-Fernández MV, Rodríguez-Castro Y. Sex education in the spotlight: what is working? Systematic review. Int J Environ Res Public Health 2021; 18: 2555. DOI: 10.3390/ijerph18052555.
50.
Beattie TS, Bhattacharjee P, Suresh M, Isac S, Ramesh B, Moses S. Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. J Epidemiol Community Health 2012; 66 Suppl 2: ii42-ii8. DOI: 10.1136/jech-2011-200475.
51.
Su R, Guo L, Tang H, Ye P, Zhang S, Xiao Y, et al. Comprehensive sexuality education weakens the effect of in-group bias on trust and fairness. Sex Educ 2020; 20: 33-45.
52.
Chi X, Hawk ST, Winter S, Meeus W. The effect of comprehensive sexual education program on sexual health knowledge and sexual attitude among college students in Southwest China. Asia Pac J Public Health 2015; 27: NP2049-NP2066. DOI: 10.1177/1010539513475655.
53.
Wang B, Hertog S, Meier A, Lou C, Gao E. The potential of comprehensive sex education in China: findings from suburban Shanghai. Int Fam Plan Perspect 2005; 31: 63-72.
54.
Wang B, Meier A, Shah I, Li X. The impact of a community-based comprehensive sex education program on Chinese adolescents’ sex-related knowledge and attitudes. J HIV AIDS Prev Children Youth 2007; 7: 43-64.
55.
Lou CH, Wang B, Shen Y, Gao ES. Effects of a community-based sex education and reproductive health service program on contraceptive use of unmarried youths in Shanghai. J Adolescent Health 2004; 34: 433-440.
56.
Huang H, Ye X, Cai Y, Shen L, Xu G, Shi R, et al. Study on peer-led school-based HIV/AIDS prevention among youths in a medium- sized city in China. Int J STD AIDS 2008; 19: 342-346.
57.
Gallant M, Maticka-Tyndale E. School-based HIV prevention programmes for African youth. Soc Sci Med 2004; 58: 1337-1351.
58.
Goldfarb ES, Lieberman LD. Three decades of research: the case for comprehensive sex education. J Adolescent Health 2021; 68: 13-27.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.