REVIEW PAPER
The lived experience of HIV-positive patients during COVID‑19: a qualitative meta-synthesis
1
School of Nursing and Midwifery, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2
Iranian Research Center on Aging, Department of Aging, University of Social Welfare and Rehabiliation Sciences, Tehran, Iran
3
Department of Health in Disaster and Emergencies, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
4
Department of Public Health, Khoy University of Medical Sciences, Khoy, Iran
5
Social Determinants of Health Research Center, Non-Communicable Diseases Research Institute, Department of Health Education and Promotion, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Submission date: 2023-09-13
Final revision date: 2023-10-15
Acceptance date: 2023-10-22
Online publication date: 2025-11-18
Corresponding author
Mojtaba Fattahi Ardakani
Diseases Research Institute, Department of Health Education and Promotion, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Diseases Research Institute, Department of Health Education and Promotion, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
HIV & AIDS Review 2025;24(4):253-261
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Patients infected with human immunodeficiency virus (HIV) face additional challenges due to the COVID-19 pandemic spreading. It is crucial to perform a qualitative synthesis to gather, evaluate, and combine the existing qualitative findings as evidence for developing interventions. Therefore, this review aimed to present the experience of HIV-infected patients during the COVID-19 pandemic.
Material and Methods:
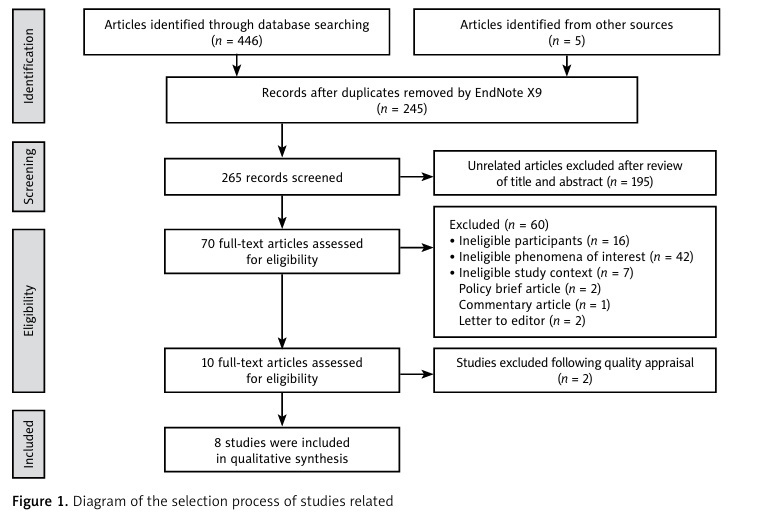
Meta-aggregation approach enabled the analysis of studies published in English between January 2020 and July 2023, while methodological quality of studies was evaluated using Joanna Briggs Institute (JBI) qualitative assessment and review instrument. Dependability and credibility of synthesized findings were assessed with ConQual guide. Five thematic content analyses and three phenomenological studies with an overall quality score of 70-100% were included.
Results:
The effective synthesis and aggregation of research findings from 213 participants in the eligible studies resulted in three distinct categories. Psychological distress, HIV care management, and social support were the three composite categories obtained from the results of qualitative studies. The ConQual score showed that two synthesized findings had a moderate rating.
Conclusions:
Overall, patients with HIV were challenged due to the advent of COVID-19, including psychological distress and the need for customized disease management. These issues call for heightened support from society and healthcare professionals.
Patients infected with human immunodeficiency virus (HIV) face additional challenges due to the COVID-19 pandemic spreading. It is crucial to perform a qualitative synthesis to gather, evaluate, and combine the existing qualitative findings as evidence for developing interventions. Therefore, this review aimed to present the experience of HIV-infected patients during the COVID-19 pandemic.
Material and Methods:
Meta-aggregation approach enabled the analysis of studies published in English between January 2020 and July 2023, while methodological quality of studies was evaluated using Joanna Briggs Institute (JBI) qualitative assessment and review instrument. Dependability and credibility of synthesized findings were assessed with ConQual guide. Five thematic content analyses and three phenomenological studies with an overall quality score of 70-100% were included.
Results:
The effective synthesis and aggregation of research findings from 213 participants in the eligible studies resulted in three distinct categories. Psychological distress, HIV care management, and social support were the three composite categories obtained from the results of qualitative studies. The ConQual score showed that two synthesized findings had a moderate rating.
Conclusions:
Overall, patients with HIV were challenged due to the advent of COVID-19, including psychological distress and the need for customized disease management. These issues call for heightened support from society and healthcare professionals.
REFERENCES (36)
1.
Ciotti M, Ciccozzi M, Terrinoni A, Jiang WC, Wang CB, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci 2020; 57: 365-388.
2.
Ioannidis JP. Global perspective of COVID‐19 epidemiology for a full‐cycle pandemic. Eur J Clin Invest 2020; 50: e13423. DOI: 10.1111/eci.13423.
3.
Bodrud-Doza M, Shammi M, Bahlman L, Islam ARMT, Rahman MM. Psychosocial and socio-economic crisis in Bangladesh due to COVID-19 pandemic: a perception-based assessment. Front Public Health 2020: 8: 341. DOI: 10.3389/fpubh.2020.00341.
4.
Jebril N. World Health Organization declared a pandemic public health menace: a systematic review of the coronavirus disease 2019 “COVID-19”. Int J Psychosoc Rehabil 2020; 24: 9160-9166.
5.
Carda S, Invernizzi M, Bavikatte G, Bensmaïl D, Bianchi F, Deltombe T, et al. The role of physical and rehabilitation medicine in the COVID-19 pandemic: the clinician’s view. Ann Phys Rehabil Med 2020; 63: 554-556.
6.
Fodjo JNS, de Moura Villela EF, Van Hees S, Dos Santos TT, Van holder P, Reyntiens P, et al. Impact of the COVID-19 pandemic on the medical follow-up and psychosocial well-being of people living with HIV: a cross-sectional survey. J Acquir Immune Defic Syndr 2020; 85: 257-262.
7.
Pantelic M, Martin K, Fitzpatrick C, Nixon E, Tweed M, Spice W, et al. “I have the strength to get through this using my past experiences with HIV”: findings from a mixed-method survey of health outcomes, service accessibility, and psychosocial wellbeing among people living with HIV during the Covid-19 pandemic. AIDS Care 2022; 34: 821-827.
8.
Garcia MO, Lumitaxi FE, Llumitaxi MG. Case study of patients with HIV during the COVID-19 pandemic. J Pure Appl Microbiol 2022; 16: 3-9.
9.
Mukamba N, Sharma A, Mwamba C, Nyirenda H, Foloko M, Lumbo K, et al. HIV care experiences and health priorities during the first wave of COVID-19: clients’ perspectives – a qualitative study in Lusaka, Zambia. BMC Public Health 2022; 22: 2238. DOI: 10.1186/s12889-022-14493-y.
10.
Feldman MS, Bell J, Berger MT. Gaining Access: a Practical and Theoretical Guide for Qualitative Researchers. Rowman Altamira; 2004.
11.
Baim-Lance A, Angulo M, Chiasson MA, Lekas HM, Schenkel R, Villarreal J, et al. Challenges and opportunities of telehealth digital equity to manage HIV and comorbidities for older persons living with HIV in New York State. BMC Health Serv Res 2022; 22: 609. DOI: 10.1186/s12913-022-08010-5.
12.
Parisi CE, Varma DS, Wang Y, Vaddiparti K, Ibañez GE, Cruz L, et al. Changes in mental health among people with HIV during the COVID-19 pandemic: qualitative and quantitative perspectives. AIDS Behav 2022; 26: 1980-1991.
13.
Seers K. What is a qualitative synthesis? Evid Based Nurs 2012; 15: 101. DOI: 10.1136/ebnurs-2012-100977.
14.
Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009; 9: 59. DOI: 10.1186/1471-2288-9-59.
15.
Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch 2006; 13: 29.
16.
Finfgeld‐Connett D. Generalizability and transferability of meta-synthesis research findings. J Adv Nurs 2010; 66: 246-254.
17.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014; 89: 1245-1251.
18.
Jobin P, Turale S. Choosing the right qualitative approach: is phenomenography a design for my study? Pac Rim Int J Nurs Res 2019; 23: 314-319.
19.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45. DOI: 10.1186/1471-2288-8-45.20. Munn Z, Porritt K, Lockwood C, Aromataris E, Pearson A. Esta.
20.
blishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol 2014; 14: 108. DOI: 10.1186/1471-2288-14-108.
21.
Munn Z, Dias M, Tufanaru C, Porritt K, Stern C, Jordan Z, et al. The “quality” of JBI qualitative research synthesis: a methodologi.
22.
cal investigation into the adherence of meta-aggregative systematic reviews to reporting standards and methodological guidance. JBI Evid Synth 2021; 19: 1119-1139.
23.
Ardakani MF, Farajkhoda T, Mehrabbeik A. Lived experiences of recovered COVID-19 patients after hospitalization: a phenomenological research. Iran J Nurs Midwifery Res 2022; 27: 308-316.23. Chiaravalloti ND, Amato MP, Brichetto G, Chataway J, Dalgas U, DeLuca J, et al. The emotional impact of the COVID-19 pandemic on individuals with progressive multiple sclerosis. J Neurol 2021; 268: 1598-1607.
24.
Natale P, Zhang J, Scholes-Robertson N, Cazzolli R, White D, Wong G, et al. The impact of the COVID-19 pandemic on patients with CKD: systematic review of qualitative studies. Am J Kidney Dis 2023; 82: 395-409.e1. DOI: 10.1053/j.ajkd.2023.04.001.
25.
Derbew Kassie T, Wasihun Y, Aschale A, Ambaw F. Lived experience of people on anti-retroviral therapy in the context of COVID-19: a phenomenological study. PLoS One 2023; 18: e0286292. DOI: 10.1371/journal.pone.0286292.
26.
Lambrinou E, Hansen TB, Beulens JW. Lifestyle factors, self-management and patient empowerment in diabetes care. Eur J Prev Cardiol 2019; 26 (2 Suppl): 55-63. DOI: 10.1177/2047487319885455.
27.
Chee SY. COVID-19 pandemic: the lived experiences of older adults in aged care homes. Millennial Asia 2020; 11: 299-317.
28.
Kardashian A, Wilder J, Terrault NA, Price JC. Addressing social determinants of liver disease during the COVID‐19 pandemic and beyond a call to action. Hepatology 2021; 73: 811-820.
29.
Galica J, Liu Z, Kain D, Merchant S, Booth C, Koven R, et al. Coping during COVID-19: a mixed methods study of older cancer survivors. Support Care Cancer 2021; 29: 3389-3398.
30.
Trenta AM, Ausili D, Caruso R, Arrigoni C, Moro M, Nania T, et al. Living with heart failure during the COVID-19 pandemic: an interpretative phenomenological analysis. Clin Nurs Res 2021; 30: 1071-1078.
31.
Radhakrishnan K, Allen C, DeMain AS, Park L. Impact of COVID-19 on heart failure self-care: a qualitative study. J Cardiovasc Nurs 2021; 36: 609-617.
32.
Bleasdale J, Leone LA, Morse GD, Liu Y, Taylor S, Przybyla SM. Socio-structural factors and HIV care engagement among people living with HIV during the COVID-19 pandemic: a qualitative study in the United States. Trop Med Infect Dis 2022; 7: 259. DOI: 10.3390/tropicalmed7100259.
33.
Devlin SA, Johnson AK, McNulty MC, Joseph OL, Hall A, Ridgway JP. “Even if I’m undetectable, I just feel like I would die”: a qualitative study to understand the psychological and socioeconomic impacts of the COVID-19 pandemic on women living with HIV (WLWH) in Chicago, IL. BMC Womens Health 2022; 22: 218. DOI: 10.1186/s12905-022-01812-z.
34.
Sharma BB, Small E, Okumu M, Mwima S, Patel M. Addressing the syndemics of HIV, mental health, and COVID-19 using the health and human rights framework among youth living with HIV, in Uganda: an interpretive phenomenological study. J Hum Rights Soc Work 2022; 7: 285-298.
35.
Fauk NK, Gesesew HA, Seran AL, Ward PR. Barriers to access to antiretroviral therapy by people living with HIV in an Indonesian remote district during the COVID-19 pandemic: a qualitative study. BMC Infect Dis 2023; 23: 296. DOI: 10.1186/s12879-023-08221-z.
36.
Linnemayr S, Jennings Mayo-Wilson L, Saya U, Wagner Z, Mac- Carthy S, Walukaga S, et al. HIV care experiences during the COVID-19 pandemic: mixed-methods telephone interviews with clinic-enrolled HIV-infected adults in Uganda. AIDS Behav 2021; 25: 28-39.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.