CASE REPORT
Opportunistic infection mimicking COVID-19 in TB/HIV-coinfected patient: a case study
1
Department of Pulmonology and Respiratory Medicine, Brawijaya University, Malang, Indonesia
Submission date: 2023-07-28
Acceptance date: 2023-09-22
Online publication date: 2025-10-20
Corresponding author
Anthony Christanto
Department of Pulmonology and Respiratory Medicine, Brawijaya University, Malang, Indonesia
Department of Pulmonology and Respiratory Medicine, Brawijaya University, Malang, Indonesia
HIV & AIDS Review 2025;24(4):334-336
KEYWORDS
TOPICS
ABSTRACT
Coronavirus disease (COVID-19) and pulmonary tuberculosis (TB) can both emerge with similar clinical presentations. Despite their different nature of progressivity, both diseases may show similarity in an acute manner, especially in the presence of secondary infection, e.g., TB. This is particularly substantial in TB/HIV-coinfection, with a myriad of possible secondary infections and different clinical presentations. These includes diagnostically challenging Pneumocystis carinii pneumonia (PCP), one of the most common opportunistic infections in TB/HIV patients.
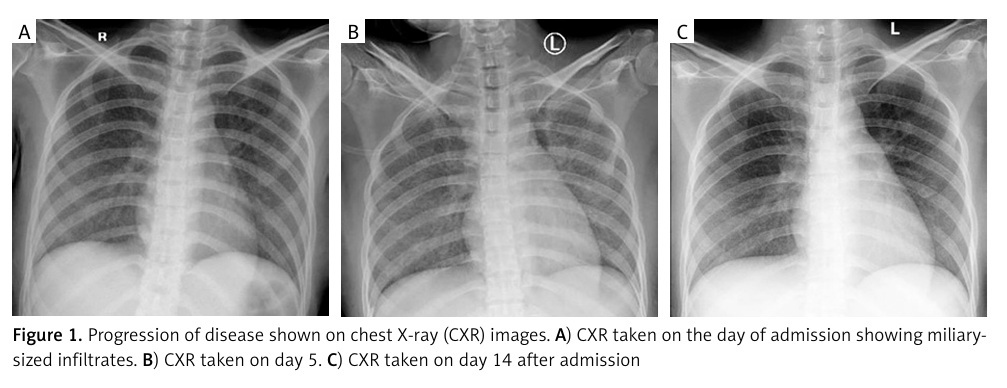
Here, we reported a case of an opportunistic infection mimicking COVID-19 in a TB/HIV-infected patient. A 22-year-old female presented to our hospital with decreased consciousness, shortness of breath, and cough. Lab results showed lymphocytopenia and thrombocytopenia as well as elevated C-reactive protein, D-dimer, and ferritin, which is classically suggestive of COVID-19 infection. She was diagnosed with probable COVID-19, but two subsequent consecutive RT-PCR tests for SARS-CoV-2 were negative. Both sputum GeneXpert MTB rapid molecular test and HIV immuno-serology rapid test were positive, and chest X-ray showed bilateral miliary infiltrates. Therefore, the patient was diagnosed as TB/HIV with secondary opportunistic infection.
As both COVID-19 and TB/HIV with opportunistic infections can present similarly debilitating risk for the patient, we highlight the importance of accurate history-taking and rapid RT-PCR test for SARS-CoV-2 to ensure accurate and timely diagnosis.
REFERENCES (16)
1.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497-506.
2.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507-513.
3.
Uyaroğlu OA, Başaran NÇ, Özişik L, Inkaya AC, Güven GS. COVID-19 at first glance, pulmonary tuberculosis with a glance in depth. Journal of Emergency Medicine Case Reports 2020; 12: 22-24.
4.
Sulis G, Roggi A, Matteelli A, Raviglione MC. Tuberculosis: epidemiology and control. Mediterr J Hematol Infect Dis 2014; 6: e2014070. DOI: 10.4084/MJHID.2014.070.
5.
García JI, Mambuque E, Nguenha D, Vilanculo F, Sacoor C, Sequera VG, et al. Mortality and risk of tuberculosis among people living with HIV in whom TB was initially ruled out. Sci Rep 2020; 10: 15442. DOI: 10.1038/s41598-020-71784-3.
6.
Oliva VM, Cezário GAG, Cocato RA, Marcondes-Machado J. Pulmonary tuberculosis: hematology, serum biochemistry and the relation with the disease duration. J Venom Anim Toxins Incl Trop Dis 2008; 14: 71-81.
7.
Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta 2020; 510: 475-482.
8.
Mandal SK, Chavan L. Erythrocyte sedimentation rate values in cases of active tuberculosis without HIV co-infection. J Med Sci Clin Res 2016; 4: 13156-13159.
9.
Akbar H, Kahloon R, Akbar S, Kahloon A. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection mimicking as pulmonary tuberculosis in an inmate. Cureus 2020; 12: e8464. DOI: https://doi.org/10.7759/cureus....
10.
World Health Organization. Global tuberculosis report 2021. Available at: https://www.who.int/publicatio....
11.
Ata F, Hussein MS, Mismar AY, Sharma R, Bozom IA, Ibrahim ZA, Ibrahim WH. Rifampicin-induced pneumonitis mimicking severe covid-19 pneumonia infection. Am J Case Rep 2020; 21: e927586. DOI: 10.12659/AJCR.927586.
12.
Asmarawati TP, Putranti A, Rachman BE, Hadi U. Opportunistic infection manifestation of HIV-AIDS patients in Airlangga university hospital Surabaya. In: IOP Conference Series: Earth and Environmental Science 2018; 125: 012061. DOI: 10.1088/1755-1315/125/1/012061.
13.
Sheikholeslami MF, Sadraei J, Farnia P, Moghadam MF, Kochak HE. Co-infection of Mycobacterium tuberculosis and Pneumocystis jirovecii in the Iranian patients with human immunodeficiency virus. Jundishapur Journal of Microbiology 2015; 8: e17254. DOI: 10.5812/jjm.17254.
14.
Catherinot E, Lanternier F, Bougnoux ME, Lecuit M, Couderc LJ, Lortholary O. Pneumocystis jirovecii pneumonia. Infect Dis Clin 2010; 24: 107-138.
15.
Tasaka S. Recent advances in the diagnosis and management of Pneumocystis pneumonia. Tuberc Respir Dis 2020; 83: 132-140.
16.
Watanabe T, Yasuoka A, Tanuma J, Yazaki H, Honda H, Tsukada K, et al. Serum (1→ 3) β-d-glucan as a noninvasive adjunct marker for the diagnosis of Pneumocystis pneumonia in patients with AIDS. Clin Infect Dis 2009; 49: 1128-1131.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.